According to the Centers for Disease Control and Prevention, more than 650,000 Americans survive a stroke every year and can be left with a variety of deficits that can challenge their independence and ability to perform activities of daily living. However, post-stroke rehabilitation services such as physical and occupational therapy, speech therapy and more can play a critical role in helping to restore functionality.
In the following interview, Allan Perel, MD, chief of neurology, and Kristine Delgado, administrative director of Rehabilitation at Staten Island-based Richmond University Medical Center, discuss the range of services offered for post-stroke patients at the hospital’s Rehabilitation Center and the impact they can have on the patient’s recovery.
What damage can a stroke do to an individual and, subsequently, what post-stroke services are typically required?
Dr. Perel: 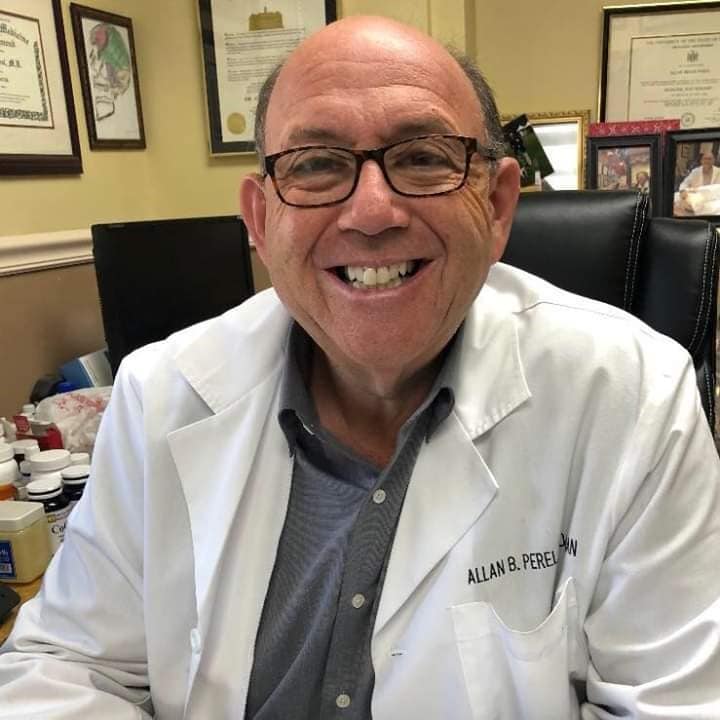 Different parts of the brain control different bodily functions, and strokes — whether they’re small, medium, large or very large — can impact multiple areas. Strokes can affect speech, cognition and motor function, so patients can experience everything from weakness or paralysis of limbs, vision issues and speech challenges to difficulty walking, driving, feeding and dressing themselves, swallowing, balancing and more. Other common fallouts of a stroke can include memory issues as well as feelings of disorientation regarding their left and right sides and where they are in space. Patients recover from strokes in a broad range of ways, often based on where the stroke occurred and the functions that were affected; sometimes a small stroke in a critical place can result in a poor prognosis while a large stroke in a less critical space won’t result in major deficits.
Different parts of the brain control different bodily functions, and strokes — whether they’re small, medium, large or very large — can impact multiple areas. Strokes can affect speech, cognition and motor function, so patients can experience everything from weakness or paralysis of limbs, vision issues and speech challenges to difficulty walking, driving, feeding and dressing themselves, swallowing, balancing and more. Other common fallouts of a stroke can include memory issues as well as feelings of disorientation regarding their left and right sides and where they are in space. Patients recover from strokes in a broad range of ways, often based on where the stroke occurred and the functions that were affected; sometimes a small stroke in a critical place can result in a poor prognosis while a large stroke in a less critical space won’t result in major deficits.
Delgado: One thing I’ve learned in my years of treating stroke patients is that each patient is so different; so many factors affect the prognosis, even among two patients who had the same-sized stroke in the same location. Our team consists of a rehab physician, or physiatrist, who leads our various therapists and determines the patient’s treatment plan based on the issues they have and their need for therapy. For example, our physical therapists would be engaged if the patient has problems with motor/sensory issues and would work with them on movement, balance and exercises to strengthen their muscles and regain their range of motion. Our occupational therapists help people relearn skills for daily living (such as grooming, preparing meals, getting dressed, driving, going back to work, etc.) and also address visual deficits, weakness in upper extremities, and cognitive skills involving insight, memory and problem-solving. Our speech pathologists treat such speech-related issues as aphasia, dysarthria (slurred speech), apraxia (difficulty with lip, jaw and tongue movements), swallowing, cognition and language-related skills such as use of the right words in the right order.
One thing I’ve learned in my years of treating stroke patients is that each patient is so different; so many factors affect the prognosis, even among two patients who had the same-sized stroke in the same location. Our team consists of a rehab physician, or physiatrist, who leads our various therapists and determines the patient’s treatment plan based on the issues they have and their need for therapy. For example, our physical therapists would be engaged if the patient has problems with motor/sensory issues and would work with them on movement, balance and exercises to strengthen their muscles and regain their range of motion. Our occupational therapists help people relearn skills for daily living (such as grooming, preparing meals, getting dressed, driving, going back to work, etc.) and also address visual deficits, weakness in upper extremities, and cognitive skills involving insight, memory and problem-solving. Our speech pathologists treat such speech-related issues as aphasia, dysarthria (slurred speech), apraxia (difficulty with lip, jaw and tongue movements), swallowing, cognition and language-related skills such as use of the right words in the right order.
What is Richmond University Medical Center’s approach to post-stroke rehabilitation?
Dr. Perel: A stroke leaves part of the brain permanently nonfunctional, so rehab is much like re-circuiting a computer and early intervention is critical. We see stroke patients for rehab therapy within 24 hours of entering the hospital and do as much as we can early on, including getting them up and around to the extent that they can. There can also be pain associated with a stroke in the form of stiff or tight muscles if they’re unable to move or turn their limbs or torso, so we offer a variety of medications to help loosen up their limbs and manage their pain. Rehab therapy is crucial because patients can continue to improve for months and years, making rehab an important investment of time and effort that they need to be involved in, and we also want them to build a strong foundation to help prevent another stroke from occurring on weakened muscles. At the same time, there’s a high incidence of post-stroke depression, so our rehab team works diligently to keep our patients’ spirits up, which is so critical.
Delgado: We see stroke patients in the hospital within 24 hours to get their rehab regimen underway and we typically see outpatients two to three times a week for 30 minutes per discipline (physical, occupational, and/or speech therapy). Our job is to identify when patients are plateauing and no longer making progress here; we provide all patients with “carryover” — exercises, tools and support they can employ on their own to continue improving at home — and teach their caregiver(s) the strategy we’re using or how they can help. We also encourage patients to follow up with their physicians and contact us if anything gets worse; they can always come back and we can work on those skills again (the earlier, the better). Post-stroke support groups are also very beneficial and, while ours were curtailed during the pandemic, we’re planning to restart them again in the hospital soon.

What final messages can you share about the importance of post-stroke rehab services and Richmond University Medical Center’s strength in this area?
Dr. Perel: Stroke can affect anyone, but having a stroke isn’t a death sentence; patients who are motivated and play an active role in their recovery, start early, and whose families are educated and participatory can do well. We love when patients surprise us and do even better than we expect — that hard work and positive attitude are so crucial.
Delgado: We have an outstanding team of therapists, many of whom are stroke-certified, and we take a team approach and collaborate with the referring physician to work with patients as a whole, which isn’t always the case with other outpatient rehab providers. We really get to know our patients and they become like family. Many times, I’ve seen our whole staff cheering when a patient reaches a milestone. I’ve seen the benefits of therapy, especially if the patient is motivated. We always try our very best to help them, and if we can’t restore function, we provide a compensation for their deficit, such as a wheelchair if they can’t walk, modified food textures if they have trouble chewing or swallowing, or an assistive device for communication if they have difficulty with speech. We get them back to functioning as best as they can so that they can participate in life as much as possible and we provide counseling as well to prepare them to tackle life situations. It’s so important for patients to come and participate in their post-stroke rehab — with our team approach and all of the knowledge and experience that our specialists bring to the rehab process, we’ve seen some great outcomes.
Richmond University Medical Center is located at 355 Bard Ave. and can be reached at 844-934-CARE or by visiting rumcsi.org. Richmond University Medical Center’s comprehensive Rehabilitation Center is located at 288 Kissel Ave.(behind the main hospital building). For more information, call 718-818-3163 or visit rumcsi.org/services/rehabilitation.
— Susan Bloom